How do I update a patient’s profile?
The first time that a patient signs in to Patient access, they are required to update their profile. The patient updates their profile and account information, and then selects Update. To update a profile at any time, or to sign out, select the user menu to view the profile and account information.
How secure is patient access?
Your details and information are protected by the highest standards of online security, so all you need to worry about is what to do with the spare time you've earnt. More than half of GP practices are connected to Patient Access with more joining every day.
How do I sign up for patient access?
The Patient Access app is available on the iOS and Android app stores for free. You can also access the website at www.patientaccess.com. You will need to register for Patient Access either online, if your practice allow this, or by asking for a registration letter from your practice.
Are there any changes to the interoperability and patient access policies?
Please review the relevant FAQs for details. As of July 1, 2021, two of the policies from the May 2020 Interoperability and Patient Access final rule are now in effect. On April 30, 2021, the requirements for hospitals with certain EHR capabilities to send admission, discharge and transfer notifications to other providers went into effect.

How do you update Patient Access?
Change account detailsSelect your name in the top right hand corner.Select Account. ... In the Sign in details section, next to Mobile Number, select Verify.Edit or add your email address and/or phone number accordingly.Enter your existing password to confirm the changes.Select Save changes.
What is the interoperability and Patient Access final rule?
The Interoperability and Patient Access final rule (CMS-9115-F) put patients first by giving them access to their health information when they need it most, and in a way they can best use it.
How can Patient Access be improved?
Five Steps to Improving Patient Access to Healthcare#1: Create a Patient Access Task Force. ... #2: Assess Barriers to Patient Access. ... #3: Turn Access Barriers into Opportunities. ... #4: Implement an Improved Patient Access Plan. ... #5: Scale and Sustain Better Patient Access.
Is MyGP same as Patient Access?
Other similar apps are Patient Access and the NHS app. You may have recently received a text message about the new MyGP App that is available to our patients. The Patient Access App is still working, MyGP is just another alternative available for our patients to use if they wish.
What is a CMS Final Rule?
CMS is issuing a final rule that advances CMS' strategic vision of expanding access to affordable health care and improving health equity in Medicare Advantage (MA) and Part D through lower out-of-pocket prescription drug costs and improved consumer protections.
What are interoperability requirements?
A definition of interoperability is "the ability to share information and services". Defining the degree to which the information and services are to be shared is a very useful architectural requirement, especially in a complex organization and/or extended enterprise.
What are the 4 barriers to accessing health services?
The study shows that lack of transport, availability of services, inadequate drugs or equipment, and costs, are the four major barriers for access.
Why is patient access important?
Patient Access often sets the tone for the patient's perception of the organization and their overall care journey. Consumers of health care are looking for the same conveniences, access to information and customer service that they are used to from other industries, such as retail and travel.
How can you improve accessibility of patient information particularly between providers?
4 Best Practices for Improving Patient-Provider CommunicationBe clear about using the patient portal.Open lines of communication using health IT.Include the patient in care coordination.Be empathetic toward the patient.
Does Patient Access still work?
Yes. You can quickly and securely give temporary access to your medical record. The shared record will be available for 24 hours via a unique link and secured using an access code. The option to Share Record , is under Medical Record on the dashboard.
Who owns Patient Access app?
Egton Medical Information Systems LimitedPATIENT ACCESS is provided by Egton Medical Information Systems Limited ("EMIS"), a company registered in England with company number 2117205 with a registered office address of Fulford Grange, Micklefield Lane, Rawdon, Leeds, LS19 6BA. The Patient Access Marketplace is also provided by EMIS.
Is the myGP app safe?
myGP is a patient-facing service that is approved by the NHS. Any data that you enter is controlled by you and hosted in a safe and secure environment.
What is interoperability in the military?
Interoperability refers to the ability of different military organisations to conduct joint operations. These organisations can be of different nationalities or different armed services (ground, naval and air forces) or both. Interoperability allows forces, units or systems to operate together.
What is Medicare interoperability?
Beginning in 2011, the Promoting Interoperability (formerly the Medicare and Medicaid EHR Incentive Programs) were developed to encourage eligible professionals (EPs) and eligible hospitals and critical access hospitals (CAHs) to adopt, implement, upgrade (AIU), and demonstrate meaningful use of certified electronic ...
What is healthcare interoperability?
Interoperability is the ability of two or more systems to exchange health information and use the information once it is received. It will take time for all types of health IT to be fully interoperable.
Why is interoperability important in healthcare?
Medical errors can prove to be fatal but interoperability allows healthcare organizations to prevent medical errors. This is because it streamlines data sharing across different applications and systems.
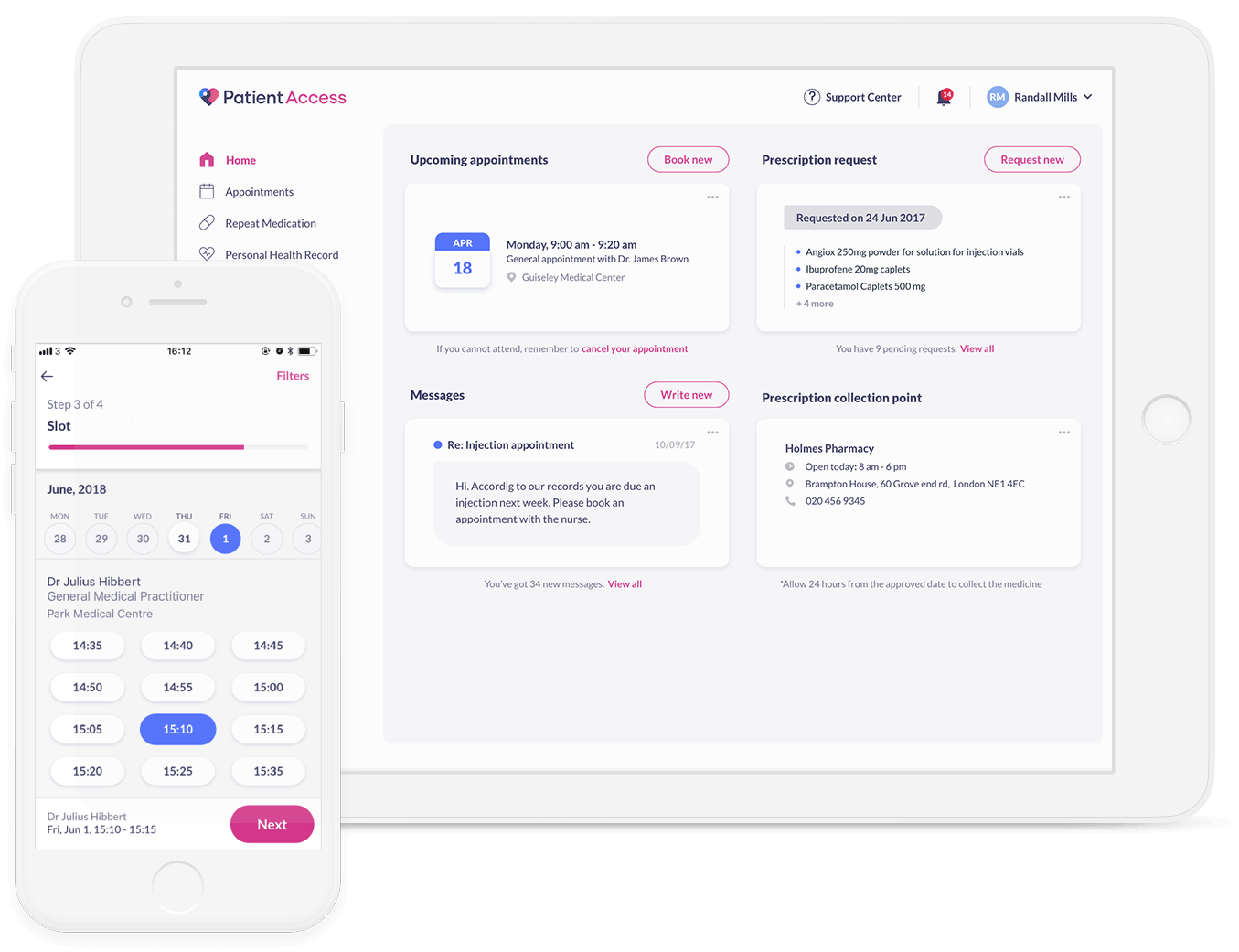
What is patient access?
Patient Access connects you to local health services when you need them most. Book GP appointments, order repeat prescriptions and discover local health services for you or your family via your mobile or home computer.
Is patient access available in the UK?
Patient Access is now available to any UK patient. Join today and benefit from a faster, smarter way to manage your healthcare.
How to keep patient information secure?
There is no single security solution that can be used to secure patient information. To keep patient information secure you need to implement layered defenses – A range of protective mechanisms that slow down any potential attack and make data access much more difficult. This is often referred to as defense in depth.
How Can You Secure Patient Information?
HIPAA requires healthcare organizations and their business associates to implement safeguards to ensure the confidentiality, integrity, and availability of PHI, although there is little detail provided on how to secure patient information in HIPAA regulations.
What is HIPAA compliant?
A secure (HIPAA-compliant) messaging platform that encrypts all communications. An intrusion detection system that monitors for file changes and irregular network activity. Auditing solutions that monitor for improper accessing of patient information.
What are the security measures that can be implemented as part of a layered security strategy?
Typical security measures that can be implemented as part of a layered security strategy include: A firewall to prevent unauthorized individuals from accessing your network and data. A spam filter to block malicious emails and malware. An antivirus solution to block and detect malware on your system.
What is vulnerability scanning?
Vulnerability scanning and penetration testing to identify vulnerabilities before they are discovered by hackers
Can you access charts in secure locations?
Storing charts in secure locations they can only be accessed by authorized individuals
Is a simple explanation required for a patient?
In most cases a simple explanation is all that is required. Patients just want reassurance that their health information is secure and will remain confidential.
What is patient access?
Patient Access is a website and mobile app which gives you access to a range of GP services online, as well as access to your health records.
Is Patient Access free?
The Patient Access app is available on the iOS and Android app stores for free.
When will CMS enforce interoperability and patient access?
As of July 1, 2021, two of the policies from the May 2020 Interoperability and Patient Access final rule are now in effect. On April 30, 2021, the requirements for hospitals with certain EHR capabilities to send admission, discharge and transfer notifications to other providers went into effect. On July 1, 2021, CMS began to enforce requirements for certain payers to support Patient Access and Provider Directory APIs. Additional information is available on the FAQ page and in the other information available below.
What is CMS Interoperability and Patient Access Final Rule?
In August 2020, CMS released a letter to state health officers detailing how state Medicaid agencies should implement the CMS Interoperability and Patient Access final rule in a manner consistent with existing guidance. There are many provisions in this regulation that impact Medicaid and CHIP Fee-For-Service (FFS) programs, Medicaid managed care plans, and CHIP managed care entities, and this letter discusses those issues. Additionally, this letter advises states that they should be aware of the ONC’s 21st Century Cures Act final rule on information blocking. The link for the letter is:
What is FHIR release 4.0.1?
FHIR Release 4.0.1 provides the first set of normative FHIR resources. A subset of FHIR resources is normative, and future changes on those resources marked normative will be backward compatible. These resources define the content and structure of core health data, which developers to build standardized applications.
What is the 21st century cures act?
Office of the National Coordinator for Health Information Technology's (ONC) 21st Century Cures Act Final Rule. The Department of Health and Human Services (HHS) finalized technical as well as content and vocabulary standards in the ONC 21st Century Cures Act final rule, which CMS adopted to support these API policies.
What is CMS 9115-F?
The Interoperability and Patient Access final rule (CMS-9115-F) put patients first by giving them access to their health information when they need it most, and in a way they can best use it. This final rule focused on driving interoperability and patient access to health information by liberating patient data using CMS authority to regulate Medicare Advantage (MA), Medicaid, Children's Health Insurance Program (CHIP), and Qualified Health Plan (QHP) issuers on the Federally-facilitated Exchanges (FFEs).
What is CMS interoperability?
When implemented effectively, health information exchange (interoperability) can also reduce the burden of certain administrative processes, such as prior authorization.
What is the payer requirement?
Payers are required to make a patient’s claims and encounter data available via the Patient Access API.
What is patient access API?
Patient Access API: CMS-regulated payers, specifically MA organizations, Medicaid Fee-for-Service (FFS) programs, Medicaid managed care plans, CHIP FFS programs, CHIP managed care entities, and QHP issuers on the FFEs, excluding issuers offering only Stand-alone dental plans (SADPs) and QHP issuers offering coverage in the Federally-facilitated Small Business Health Options Program (FF-SHOP), are required to implement and maintain a secure, standards-based (HL7 FHIR Release 4.0.1) API that allows patients to easily access their claims and encounter information, including cost, as well as a defined sub-set of their clinical information through third-party applications of their choice. Claims data, used in conjunction with clinical data, can offer a broader and more holistic understanding of an individual’s interactions with the healthcare system, leading to better decision-making and better health outcomes. These payers are required to implement the Patient Access API beginning January 1, 2021 (for QHP issuers on the FFEs, plan years beginning on or after January 1, 2021).
What is CMS' role in protecting patient information?
CMS is taking additional steps to provide payers and patients opportunities and information to protect patient data and make informed decisions about sharing patient health information with third parties. For instance, as part of this final rule a payer may ask third-party application developers to attest to certain privacy provisions, such as whether their privacy policy specifies secondary data uses, and inform patients about those attestations. CMS is also working with payers to provide information they can use to educate patients about sharing their health information with third parties, and the role of federal partners like the Office for Civil Rights (OCR) and the Federal Trade Commission (FTC) in protecting their rights.
What is CMS data exchange?
Payer-to-Payer Data Exchange: CMS-regulated payers are required to exchange certain patient clinical data (specifically the U.S. Core Data for Interoperability (USCDI) version 1 data set) at the patient’s request, allowing the patient to take their information with them as they move from payer to payer over time to help create a cumulative health record with their current payer. Having a patient’s health information in one place will facilitate informed decision-making, efficient care, and ultimately can lead to better health outcomes. These payers are required to implement a process for this data exchange beginning January 1, 2022 (for QHP issuers on the FFEs, plan years beginning on or after January 1, 2022).
What is CMS 9115-F?
Overview#N#The Interoperability and Patient Access final rule (CMS-9115-F) delivers on the Administration’s promise to put patients first, giving them access to their health information when they need it most and in a way they can best use it. As part of the Trump Administration’s MyHealthEData initiative, this final rule is focused on driving interoperability and patient access to health information by liberating patient data using CMS authority to regulate Medicare Advantage (MA), Medicaid, CHIP, and Qualified Health Plan (QHP) issuers on the Federally-facilitated Exchanges (FFEs).
When is the provider directory API required for MA?
MA organizations, Medicaid and CHIP FFS programs, Medicaid managed care plans, and CHIP managed care entities are required to implement the Provider Directory API by January 1, 2021. QHP issuers on the FFEs are already required to make provider directory information available in a specified, machine-readable format.
When will CMS start reporting?
Digital Contact Information: CMS will begin publicly reporting in late 2020 those providers who do not list or update their digital contact information in the National Plan and Provider Enumeration System (NPPES). This includes providing digital contact information such as secure digital endpoints like a Direct Address and/or a FHIR API endpoint. Making the list of providers who do not provide this digital contact information public will encourage providers to make this valuable, secure contact information necessary to facilitate care coordination and data exchange easily accessible.
When will CMS report CAHs?
Public Reporting and Information Blocking: Beginning in late 2020, and starting with data collected for the 2019 performance year data, CMS will publicly report eligible clinicians, hospitals, and critical access hospitals (CAHs) that may be information blocking based on how they attested to certain Promoting Interoperability Program requirements. Knowing which providers may have attested can help patients choose providers more likely to support electronic access to their health information.
Who is responsible for assisting patients and accepting patient requests for amendments?
The Health Information Management (HIM) Department, Privacy Officer or designee will be responsible for assisting patients and accepting patient requests for amendments. The organization’s Privacy Officer will be responsible for processing all individual requests for amendments.
What happens if the DRS is not readable?
If the form and format of the electronic information in the DRS are not readily producible or, if not in a readable electronic form and format, then the health information may be produced by the covered entity (CE) in the form and format agreed to by the individual.
What is the HIPAA privacy rule?
The HIPAA privacy rule provides patients with specific rights to their health information. Regulations applied to covered entities (healthcare plans, healthcare clearinghouses, and healthcare providers who transmit specific transactions electronically), as well as the business associates of these organizations, established an individual’s right to access and amend their PHI in all but a limited number of situations. This includes PHI in any media (paper, electronic, or oral) that is maintained by a covered entity or its business associate. The Patients’ Right to Access must be granted within 30 days regardless of record location (onsite vs. offsite) and regardless of media type. One 30-day extension applies but must be communicated to the patient and documented. Any denial of access also needs to fit within this 30 day/60 day time frame.
What happens if another covered entity notifies this organization of an amendment to PHI it maintains?
If another covered entity notifies this organization of an amendment to PHI it maintains, the amendment will be made to this organization’s patient medical record.
What happens if a patient submits a statement of disagreement?
If the patient submitted a statement of disagreement, the organization will disclose all information listed above or an accurate summary of such information with all future disclosures of PHI to which the disagreement relates.
What is HIPAA and HITECH?
The Health Information Portability and Accountability Act (HIPAA) and then the Health Information Technology for Economic and Clinical Health Act (HITECH) changed how covered entities approach a patient’s right to access and amend Protected Health Information (PHI). Generally, all consumers now have the ability to inspect, obtain a copy, ...
Where are requests for amendments filed?
General information regarding requests for amendment, forms relating to amendments and correspondence relating to denial or acceptance of requests to amend will be filed in the patient’s designated record set and appended to the protect health information (PHI) as required by the Privacy Rule.
What is information blocking and what kind of information will patients be able to access and share?
Section 4004 of the Cures Act specifies certain practices that could constitute information blocking, which the Final Rule says would restrict patients’ access to all of their health records. There are eight exceptions to the information-blocking rule, which gives clinicians some flexibility to protect patient privacy and security and where data interoperability is not technically reasonable. Health care providers will be required to provide patients access to all health information in their electronic medical records, free of charge. To support interoperability, the new rules indicate eight types of clinical notes that must be shared with patients: consultation notes, discharge summary notes, history and physical examination, imaging narratives, laboratory report narratives, pathology report narratives, procedure notes and progress notes.
What are the eight types of clinical notes that must be shared with patients?
To support interoperability, the new rules indicate eight types of clinical notes that must be shared with patients: consultation notes, discharge summary notes, history and physical examination, ...
What is the cures act?
Signed into law in 2016, the Cures Act is intended to push the pace of innovation of drugs, biological products and medical devices in order to empower patients. The new rules, published last year, implement a portion of the Cures Act regarding health information technology improvements.
When will optometry change to 21st century?
January 7, 2021. Under new rules for the 21st Century Cures Act, doctors of optometry will need to prepare for changes going into effect April 5. Doctors should check in with their health IT vendor in order to make sure they meet the new requirements. Is your practice ready for new measures empowering patients with greater access ...
How is the final rule different than the Health Insurance and Portability and Accountability Act (HIPAA)?
The Cures Act Final Rule pertains exclusively to electronic health information and the access and exchange of that electronic data. That sets it apart from HIPAA, which covers paper, electronic and verbal data as protected health information.
How does the Cares Act affect HIPAA?
The CARES Act improves 42 CFR Part 2 regulations by expanding the ability of healthcare providers to share the records of individuals with SUD, but also tightens the requirements in the event of a breach of confidentiality. In short, the changes made by the CARES Act have aligned 42 CFR Part 2 regulations more closely with HIPAA.
What happened to HIPAA in 2019?
One notable HIPAA change that happened in 2019 was an update to the penalties for noncompliance, which were reduced in three of the four penalty tiers. The HITECH Act called for an increase in penalties for noncompliance with HIPAA.
How are New HIPAA Regulations Introduced?
Before any regulations are changed, the Department of Health and Human Services seeks feedback on aspects of HIPAA regulations that are proving problematic or, due to changes in technologies or practices, are no longer as important as when they were signed into law.
What does the Department of Health and Human Services do before changing HIPAA regulations?
Before any regulations are changed, the Department of Health and Human Services seeks feedback on aspects of HIPAA regulations which are proving problematic or, due to changes in technologies or practices, are no longer as important as when they were signed into law.
How long does it take to get a SUD notified?
The same breach notification requirements as HIPAA will apply, so any data breach will require the patient to be notified without unnecessary delay, and no later than 60 days from the discovery of the breach.
When did HIPAA change?
Tt has been several years since new HIPAA regulations have been introduced but that is likely to change very soon. The last update to the HIPAA Rules was the HIPAA Omnibus Rule changes in 2013, which introduced new requirements mandated by the Health Information Technology for Economic and Clinical Health (HITECH) Act. There are, however, expected to be several 2021 HIPAA changes as OCR has issued a Notice of Proposed Rulemaking in December 2020 that outlines several changes to the HIPAA Privacy Rule.
What is the Cares Act?
The CARES Act improves 42 CFR Part 2 regulations by expanding the ability of healthcare providers to share the records ...