As part of our FY 2013 Audit Plan, we completed the Patient Access Audit, which specifically focused on patient registration and insurance verification processes. The objective of the audit was to determine whether patient registration processes and systems are adequate to support timely, accurate and efficient billing.
Full Answer
How does patient access affect revenue cycle?
Patient access is the starting point for your entire revenue cycle process. Ensuring correct patient information on the front end reduces the errors that cause rework in the back office. 10 to 20 percent of a health system's revenue is forced to remediate denied medical claims and 30 to 50 percent of those occur during patient access.
What is “patient access?
What patient access means to different entities For some, “patient access” refers to the clinic department that’s responsible for registration, insurance verification, cash collections, and so forth. The health system strategists define patient access quite differently.
What is in partnership with patient access?
In partnership with Patient Access connects you to local health services when you need them most. Book GP appointments, order repeat prescriptions and discover local health services for you or your family via your mobile or home computer.
What is involved in patient registration?
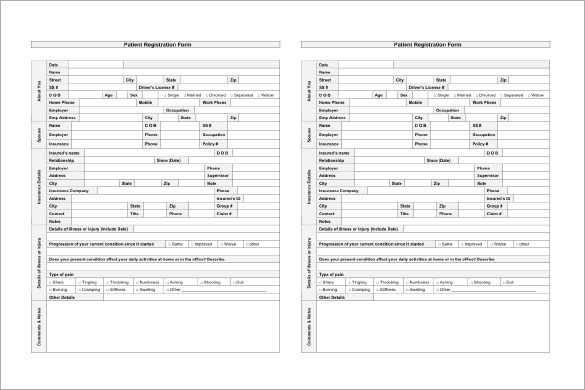
Registration: Registration is the first interface that the patient has with the health facility. In addition to validating demographic and insurance information other mandated fields are captured during patient registration.
.png?itok=DsOO403H)
Why is patient access so important?
Patient Access often sets the tone for the patient's perception of the organization and their overall care journey. Consumers of health care are looking for the same conveniences, access to information and customer service that they are used to from other industries, such as retail and travel.
What is patient access process?
In the most basic sense, patient access refers to the ability of patients and their families to take charge of their own health care. With the advent of the internet and digital marketing, medical practices and businesses have a new way to reach their target audiences.
What is Patient Access management?
As a patient access manager, you work in a hospital, overseeing the admissions and registration department. In this role, your job duties include training new staff members, enforcing health care policies, managing patient scheduling, and addressing patient concerns.
What data is collected by patient access personnel?
The data collected is utilized by multiple members across the healthcare team, to include Patient Accounts, Patient Information, Clinicians and Health Information Management. Collection of Insurance Information: The patient access department provides the input of the patients' insurance or payment information.
What is patient access NHS?
Patient Access connects you to local health services when you need them most. Book GP appointments, order repeat prescriptions and discover local health services for you or your family via your mobile or home computer. Register.
What is patient access in revenue cycle?
Patient Access is the entryway and foundation for all revenue cycle functions, and it often provides the first impression of a facility to a patient. With increasing pressure on reimbursement and the patient experience, Patient Access has a new light shining on it with no room for error.
Who is patient access?
Patient Access is a great online service which allows you to book appointments, order repeat prescriptions, view your medical records and send secure messages to the practice. The services is open 24/7/365 and can be accessed from your home PC, Tablet or Mobile phone.
How can patient access be improved?
Five Steps to Improving Patient Access to Healthcare#1: Create a Patient Access Task Force. ... #2: Assess Barriers to Patient Access. ... #3: Turn Access Barriers into Opportunities. ... #4: Implement an Improved Patient Access Plan. ... #5: Scale and Sustain Better Patient Access.
What does re-audit registration mean?
Re-audit registrations after any changes and receive alerts to warn if any updated information is still incorrect
What is the key to improving net patient revenue?
The answer to improved net patient revenue lies in your front-end processes. Denials prevention—not management—is the key to reducing bad debt, write-offs and protecting net patient revenue.
How does EngageCare improve patient registration?
EngageCare Registration Quality Assurance increases patient registration accuracy by using software and a proprietary rules engine to automatically audit 100 percent of your patient registrations, identifying hundreds of types errors. Real-time alerts on registrars’ work queues flag accounts that need corrections and deliver clear instructions to registrars of how to correct errors and submit clean claims.
What is AccuReg software?
AccuReg is the only software that embeds NAHAM’s AccessKeys ® into our patient access solution to provide hospitals with national benchmarking standards and best practices. Customized educational courses and tests serve as an evaluation tool for supervisors to view and measure staff performance.
What is patient access?
Patient access is the starting point for your entire revenue cycle process. Ensuring correct patient information on the front end reduces the errors that cause rework in the back office. 10 to 20 percent of a health system's revenue is forced to remediate denied medical claims and 30 to 50 percent of those occur during patient access.
How does automated workflow improve patient care?
By adopting an automated, data-driven workflow—not only are you reducing the errors that lead to claim denials, you’re also improving access to care for your patients through capabilities like online scheduling options that are available 24x7. Access is further improved by reducing the friction around patient billing by leveraging real-time eligibility verification to deliver accurate patient estimates at registration.
How long does it take for SDMIC to determine if a patient is eligible for insurance?
In under 30 seconds SDMIC’s staff can determine if a patient is eligible with the presented insurance. They also leverage automated patient estimates to provide price transparency to patients and accurately collect from patients in real time.
What is patient access?
Patient Access connects you to local health services when you need them most. Book GP appointments, order repeat prescriptions and discover local health services for you or your family via your mobile or home computer.
Is patient access available in the UK?
Patient Access is now available to any UK patient. Join today and benefit from a faster, smarter way to manage your healthcare.
What is the role of patient access in the revenue cycle?
The Patient Access as a core function of the Revenue Cycle starts with registration, scheduling and all of its support processes to patients, providers, and payers throughout the patient’s healthcare experience. Its main function is to supply information which results in building the foundation for medical records, billing & collections.
What is the purpose of the patient access department?
Collection of Insurance Information: The patient access department provides the input of the patients’ insurance or payment information. They scan and store multiple insurance card images and maintain a complete history of patient’s past, present and future insurances. The patient’s financial responsibility is determined by gathering data about insurance coverage, additional insurance, and their maximum allowable visits.
What is iPatientCare?
iPatientCare is a leading healthcare technology company providing Cloud-based Unified System integrating EHR, PMS and RCM technology enhancing patient care through care management/coordination/analytics, and reducing costs of care delivery At iPatientCare, we help clients address today’s evolving Patient Access needs. As a single source, we can create standardization and accountability across all of your revenue cycle operations.
What is a patient self check in kiosk?
Patient Self Check-in Kiosk: Patient kiosk is tabloid and a phone-based software application that assists patients to do self check-in and also edit their basic demographic details. Patient kiosks can be considered as the new step taken to streamline and simplify the patient registration procedure. This Patient Self Check-in Kiosk frees the front desk from manual data entry tasks and allows them to utilize their time productively.
What is the purpose of registration?
Registration: Registration is the first interface that the patient has with the health facility. In addition to validating demographic and insurance information other mandated fields are captured during patient registration. This information serves as the foundation of the patient’s medical record. The data collected is utilized by multiple members across the healthcare team, to include Patient Accounts, Patient Information, Clinicians and Health Information Management.
How does iPatientCare help?
Learn more on how iPatientCare can help you meet your challenges – from reducing bad debt to increase collections, improving efficiency and revitalize your Patient Access operations. For more information schedule a free consultation with our experts now.
How to strengthen patient access?
Generally, to strengthen the patient access, embracing technology within the revenue cycle is key. The new age of Patient Access requires better alignment to deal with key issues facing organizations and the community. The goal should be to holistically integrate Patient Access within the revenue cycle for optimal performance, focusing efforts around people, process and technology to better address client needs. Achieving the highest results requires strategies and expertise that can address the patient as an individual consumer, keeping them at the center of the process.
When did the VA do a national access audit?
In mid-April 2014, the Secretary of Veterans Affairs directed the Veterans Health Administration (VHA) to complete a nation-wide Access Audit to ensure a full understanding of VA’s policy among scheduling staff, identify any inappropriate scheduling practices used by employees regarding Veteran preferences for appointment dates, and review waiting list management.
When did the VA start accelerating access to care?
On Wednesday, May 21, 2014 VA launched the Accelerating Access to Care Initiative, a nation-wide program to ensure timely access to care. As directed by President Obama, VHA identified Veterans across the system experiencing waits that do not meet Veterans expectations for timeliness. VA began contacting and scheduling all Veterans who are waiting for care in VA clinics or arranging for care in the community, while simultaneously addressing the underlying issues that impede Veterans’ access.
Why was the Gainesville clinic incorrectly populated?
Initial data published for 1/22/2015 contained an inaccuracy for the number of appointments scheduled for the clinics under the Gainesville, FL parent facility. Due to a transcription error, the facility names listed under the Gainesville parent facility were incorrectly populated. We have corrected this transcription error and apologize for the confusion.
When did VA update completed appointments?
On October 30, 2015, VA updated Completed Appointments (As of 30 September 2015) to correct inaccuracies that resulted from recent facility name changes.
Does the 2016 enrollment list include new enrollment requests?
Initial Pending Appointments data published for May 1, 2016 did not include New Enrollee Appointment Request list totals at the national and local levels. This updated release includes these totals.
How can root cause tracking and analysis of these accounts help place focus on gaps in the process?
Patient Access operations can fill these gaps by creating and implementing policies and procedures detailing activities and results required to financially authorize an account. These policies should also define criteria for any services and/or thresholds that make it acceptable for a patient to proceed with services outside of the completion of those identified activities.
Why is it so hard to compare key indicators across hospitals?
As with any metric, comparing some key indicators across hospitals and health systems can be difficult at best due to differences in the way they are calculated and tracked - leading to an apples-and-oranges comparison. Each of these metrics below, however, can be valuable to an organization by first simply tracking internally and then focusing on performance improvements that can be compared to a hospital's historical performance to drive better results.
Why should healthcare providers understand and measure each of these time intervals separately, as well as collectively, to identify the?
Healthcare providers should understand and measure each of these time intervals separately, as well as collectively, to identify the areas with the greatest opportunities for improvement.
What are the top four denial categories for pre-service registration?
It is during the registration process that providers are most vulnerable to the top four denial categories, which include authorization, medical necessity, coding and eligibility.
