Patient access is the foundation for optimal revenue cycle performance because providing care is the primary income source for health systems. Therefore, if patients can’t easily access care, hospitals can’t deliver that care, nor generate income because patients will seek care elsewhere.
What are the steps in the revenue cycle?
Steps Included In Revenue Cycle Management
- Pre-Registration. Pre-registration allows the medical practice to capture information, insurance information, and eligibility in real-time, often while the patient is still on the phone.
- Registration. Registration is the process of ensuring the patient’s information is accurate. ...
- Charge Capture. ...
- Coverage. ...
- Claim Submission. ...
- Medical Coding. ...
- Payments. ...
What are the steps in the medical revenue cycle?
To get there, leading healthcare revenue cycle teams center their efforts on:
- Price transparency. Now more than ever, people are asking questions about the price of healthcare. ...
- Supporting equitable access to care. Revenue cycle staff assist patients with applying for financial assistance, when needed. ...
- Financial conversations with patients. ...
What is the definition of revenue cycle?
Revenue cycle The recurring set of business activities and data processing operations associated with providing goods and services to customers and collecting cash in payment for those sales What are the basic revenue cycle activities?
What is revenue cycle in hospital?
The revenue cycle management systems are intended to decrease charging mistakes by medicinal services suppliers and are broadly utilized as a part of nations, for example, the U.S. where medicinal coding process is unpredictable and dreary.

What is patient access in revenue cycle?
Patient Access is the entryway and foundation for all revenue cycle functions, and it often provides the first impression of a facility to a patient. With increasing pressure on reimbursement and the patient experience, Patient Access has a new light shining on it with no room for error.
Why is patient access a critical point in the revenue cycle process?
Through patient access, revenue cycle teams can also clear patients financially for their scheduled services by verifying information and discussing and collecting upfront patient financial responsibility, such as copayments.
What is the role of the revenue cycle in relation to healthcare?
The healthcare revenue cycle is designed to manage the complexity of hospital billing cycles, maintaining cash flow that enables healthcare facilities to deliver the maximum standard of care to patients.
Is medical records part of revenue cycle?
Maintaining proper medical records in the revenue cycle is crucial because it is such an important cross-section of what you focus on as part of your daily routine. Already more than 89 percent of physicians use EMR or electronic health records, but only 10 percent say they are satisfied with their current system.
Why is patient access so important?
Patient Access often sets the tone for the patient's perception of the organization and their overall care journey. Consumers of health care are looking for the same conveniences, access to information and customer service that they are used to from other industries, such as retail and travel.
How important is patient access?
Patient access can have a direct impact on the quality of care, and one of the most important aspects of good patient access is good communication between patients and healthcare providers. Research documents show a direct relationship between patient compliance and quality of care.
What are 4 steps in revenue cycle?
The first step in revenue cycle management is pre-authorization and registration. This is the point at which you gather the patient's insurance and financial information....Revenue Cycle Management:Step 2: Services and Charge Capture. ... Step 3: Claim Submission and Denial Management. ... Step 4: Payment. ... Step 5: Quality Reporting.
What are the key players in revenue cycle roles?
The revenue cycle touches all of the key stakeholders involved in a patient's care: the patients themselves, clinicians, providers and payors. The typical revenue cycle for a provider starts at the first point of contact with the patient.
What are the 6 stages of the revenue cycle in healthcare?
The Six stages of the revenue cycle are provision of service, documentation of service, establishing charges, preparing claim/bill, submitting claim, and receiving payment.
What is the most important part of the revenue cycle?
Preregistration is the first and most vital step in the revenue cycle process.
What are the 10 steps in the medical billing revenue cycle?
10 Steps in the Medical Billing ProcessPatient Registration. Patient registration is the first step on any medical billing flow chart. ... Financial Responsibility. ... Superbill Creation. ... Claims Generation. ... Claims Submission. ... Monitor Claim Adjudication. ... Patient Statement Preparation. ... Statement Follow-Up.More items...
What is the difference between medical billing and revenue cycle management?
Revenue Cycle Management includes the medical billing process mentioned above, but it goes way beyond invoicing and payments. It includes everything from determining patient eligibility, documenting how and when services are delivered, to coding, submitting, and managing claims and payments.
Why is patient Registration such a critical component of healthcare quizlet?
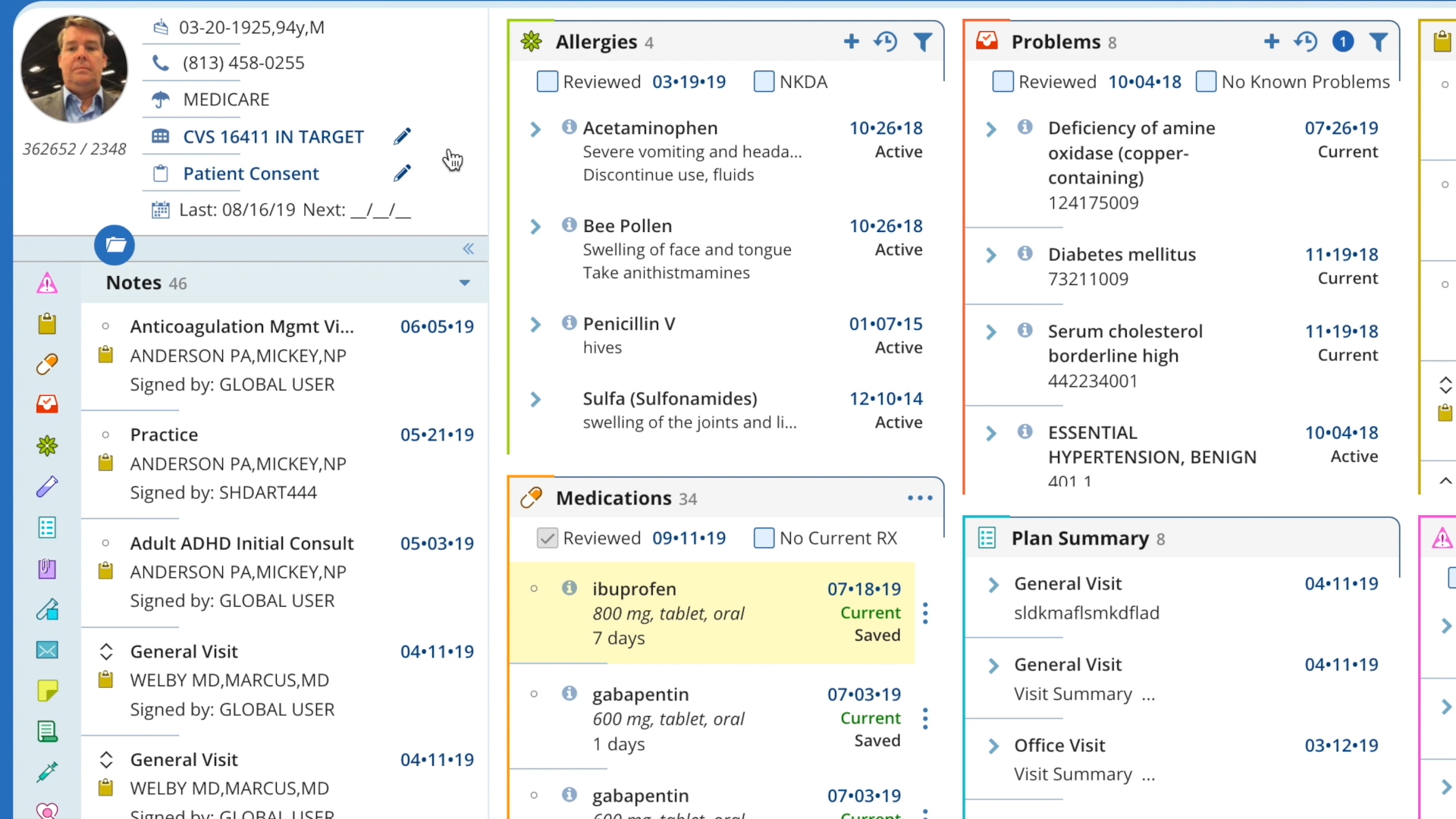
data that initiates the documentation for the patient encounter, a process called registration. called patient registration or admissions. The data collected or initiated by patient access are critical to the accurate accumulation of patient data and the timely processing of an error-free claim.
What is patient access process?
Patient Access typically involves scheduling, registration, financial clearance, and patient collection.
What are the process involved in patient access?
Patient Access ServicesSchedule Patients and obtain all patient details.Verify Insurance, and eligibility for services - determine copayment, Co-insurance and deductible levels.Determine prior authorization requirements.Register Patients- make demographic and insurance updates.
What is meant by patient access?
At its most basic, “patient access” is defined quite literally. It refers to the availability of healthcare, the ability of consumers to access care and treatment. Patient access is an integral part of the Affordable Care Act (ACA).
What percentage of revenue cycle data is gathered by patients access teams?
About 40% of data used for revenue cycle management are gathered by Patients Access Teams.
Why is patient access important?
The Patients Access plays a very important role in capturing and collection of patient service revenue.
How does delayed reimbursement affect cash flow?
Delayed reimbursement will significantly affect your cash flow. Patients satisfaction, prompt payments are the best results of your high quality customer service and are all based on how good your team with their communication skills.
What happens if you fail to verify your HMO?
Because their coverage may always change. If you fail to verify eligibility, there is a very high risk of claim denial for sure. Possible scenarios? the patient may not be eligible at the time of service, or the HMO was not contracted with your practice at that time of service. Result? claim may not get paid. Resulting in lose of revenue.
What is the data analysis for revenue cycle?
Analyze data from across your revenue cycle: Consumer effectiveness (estimations), insurance effectiveness (authorization, eligibility), and team effectiveness (time, cost to collect)
What are the priorities of a patient access department?
After ensuring a quality patient experience, two top priorities for a patient access department are to secure correct payment from insurance and from consumers. There are other priorities related to reducing the cost to collect, increasing patient volume, and boosting patient satisfaction, but payment tops the list.
How does patient access analytics help?
Patient access analytics can also help identify how efficient a provider’s patient access workflow is, and pinpoint ways it can be improved.
How can healthcare providers improve patient experience?
Healthcare providers can improve patient experience, increase point-of-service payments, and reduce denials by raising visibility into eligibility and registration processes and using root cause analysis to drive corrective action.
How to improve patient access?
Here’s an essential capabilities checklist for an analytics solution to help improve patient access performance: 1 Analyze data from across your revenue cycle: Consumer effectiveness (estimations), insurance effectiveness (authorization, eligibility), and team effectiveness (time, cost to collect) 2 Standardize your data with organizationwide reports 3 Offer a library of customizable reports aligned with your business processes 4 Automatically generate reports on your timetable 5 Provide at-a-glance visibility into performance—historical, real-time, and across facilities
What happened to a 600 bed health system?
Consider what happened to a 600-bed system that had overall denial rates substantially higher than comparable health systems. It analyzed why denial rates were so high and found that registration and eligibility issues were the primary denial causes. Based on that analysis, it targeted specific patient access processes, and the related registration/eligibility denial rate plummeted from 11.66 percent to 1.23 percent. Over a four-month period, that led to $2.4 million in revenue paid on initial submission.
What is the rise of consumerism and complexity of emerging payment models?
The rise of consumerism and complexity of emerging payment models challenge providers more than ever to secure timely and correct payment from both. And, ultimately, the success or failure of these collections begins at the front-end of the revenue cycle.
What is patient access in 2021?
May 06, 2021 - Patient access is generally the first encounter a patient will have with a healthcare organization, making it central to the patient experience. But this aspect of healthcare is also a major first for another area: revenue cycle management. During the patient access process, revenue cycle teams have their chance to get medical ...
What is the importance of ensuring patient access staff complete registration and eligibility verification?
Ensuring patient access staff complete registration and eligibility verification are key to preventing some of the most common and avoidable claim denials. But even these tasks can be a challenge for the 30 percent of health systems relying on manual patient access workflows.
What is digital transformation in Goshen Health?
The digital transformation at Goshen Health was able to alleviate many of the pain points of patient access—long wait times, inaccurate data capture, and no-shows—but it also helped to strengthen relationships between all the players involved in a patient’s healthcare journey.
What is the solution for protecting the bottom line while improving the patient experience?
Integrating traditional patient access tools with digital intake and engagement is the solution for protecting the bottom line while improving the patient experience.
Do hospitals have a second chance?
But hospitals rarely have a second chance to get things right not only with their patients but also their providers and payer partners.
Is data integrity key to revenue cycle management success?
But data integrity will be key to revenue cycle management success as patient access evolves.
How can a patient-centered access center improve revenue cycle?
When health systems prioritize patient access, they can improve the healthcare revenue cycle through decreased referral leakage, improved communication across different departments, and getting patients to the right place the first time.
Why is patient access important in healthcare?
Patient access is the foundation for optimal revenue cycle performance because providing care is the primary income source for health systems. Therefore, if patients can’t easily access care, hospitals can’t deliver that care, nor generate income because patients will seek care elsewhere. Establishing a patient-centered access center, one place (or source of truth) for all patient inquiries, requests, and referrals, can help health systems optimize patient access and, thus, improve the healthcare revenue cycle.
How can organizations improve patient access?
Advancing patient access is complex, but there are many ways organizations can achieve better access. Centralizing ownership of referrals and orders through a patient-centered access center and training access center staff to provide patients with a consistent experience, no matter where they receive care throughout the system (e.g., cardiovascular, pulmonary, orthopedics) have a positive impact on access. A decentralized approach often fails to hold team members accountable for sending referrals and orders to the right place.
Why is it important to have a patient centered access center?
Establishing a patient-centered access center, one place (or source of truth) for all patient inquiries, requests, and referrals, can help health systems optimize patient access and, thus, improve the healthcare revenue cycle.
What is decentralized patient access?
Historically, health systems have taken a decentralized patient access approach (Figure 1). This scattered approach makes it difficult for team members to follow referrals, ensure the referral makes it to the correct destination, and identify the process gap that sends a referral to the wrong place. Inconsistent responsiveness (e.g., in a decentralized call center) leads to patient confusion and dissatisfaction, increasing the likelihood that a patient will seek care elsewhere.
How can access center help health systems?
Health systems can also optimize resources by cross-training staff so that all team members at the access center can handle every type of patient access request, rather than transferring patients to other teams. For example, to overcome cancellations and no-shows, leaders can train all access center team members about the correct workflow to fill empty patient slots, giving patients every opportunity to schedule and keep an appointment. When a patient-centered access center provides every opportunity for a patient to receive care, the health system has the chance to generate revenue from those appointments instead of losing revenue from canceled or missed appointments.
What are the challenges of patient access?
Common patient access resource challenges include differing schedule management practices by department and a lack of clarity around patient cancellations and no-shows. To tackle scheduling management differences, health systems can better optimize resources by creating and distributing standard templates and protocol guidelines.
Customer Service is Engrained in the Model
At Albany Medical Center Hospital, Pallozzi has taken part in her team’s revamp and restructure from a Customer Service Program, to what today is known as the Patient Experience Module.
Having an Honest Conversation With Patients
Priming patients on the actual costs of service can be difficult, especially as the numbers we see today are becoming larger and larger. Pallozzi explains that the patient access team today bears a greater duty in being educated on various health insurance plans, deductibles, and copays.
Patient Access: A Numbers Game
While one might not immediately think of improving patient access and patient experience as being quantifiable, Pallozzi believes that it must be; “I think that what many of the patient access professionals will tell you is Chief Financial Officers - they deal with numbers.
Why do healthcare organizations need to evaluate their patient access processes and technology?
Healthcare organizations must continue to evaluate their Patient Access processes and technology to ensure everything is captured to secure payment while ensuring that patient satisfaction is achieved on every patient every time.
What happens if a patient is not scheduled for a test?
Additionally, if patients are not scheduled appropriately, there may be gaps in the department schedules.