What is medication nonadherence and how can you prevent it?
Medication nonadherence is when a patient does not take a prescribed medicine or follow the provider’s instructions for taking the medicine. Barriers that prevent patients from taking their medications can appear at the patient, provider, or health system level.
What are the barriers to patient adherence to medication?
These barriers may be complex and include factors related to socioeconomics, health care system structures and processes, severity of co-occurring medical conditions, complexity of medication and nonmedication therapies, and patient concerns. 3 Factors that affect a patient’s medication adherence may include: Medication cost.
What are the possible adverse effects of medication access problems?
69% of patients with medication access problems had adverse events compared to 40% for patients with no access problems. These adverse events include: 22% had an increase in suicidal ideation or behavior.
What is patient access and how does it work?
"Patient Access connects you to healthcare services when you need them most. Book GP appointments, order repeat prescriptions and explore your local pharmacy services.".
What are the barriers to medication adherence?
What is medication management?
What is the Joint Commission of Pharmacy Practitioners?
How does a pharmacy intervention help with CVD?
How can public health practitioners support the CPSTF recommendation?
Why is it important to recognize and convene partners involved in implementing the interventions?
Why are pharmacies using the Patient Care Process?
See 4 more
About this website

Why is access to medication important?
Reduced access to prescription medications may cause the patient to have to choose a drug less effective than the drug their doctor would prefer they have. Their conditions will not be treated as well, and a physical toll will be taken on the physical, emotional and mental well-being.
What is patient access in pharma?
Patient access is controlled by complex interactions between governmental and third-party payers, pharmacy benefit managers (PBMs), distributors, pharmaceutical manufacturers, health systems, and pharmacies that together control the receipt of goods by patients after prescription by clinicians.
What are some reasons a patient may not be compliant with their medications?
8 reasons patients don't take their medicationsFear. Fear. ... Cost. Cost. ... Misunderstanding. Misunderstanding. ... Too many medications. Too many medications. ... Lack of symptoms. Lack of symptoms. ... Mistrust. Mistrust. ... Worry. If a patient is concerned about becoming dependent on a medicine, it can also lead to nonadherence. ... Depression.
Can patients taking their own medications while in the hospital?
A survey of directors of pharmacy at small hospitals (300 beds or less) found that a majority (90.9%) of the hospitals allowed patients to use their own medications while in the hospital.
How important is patient access?
Patient access can have a direct impact on the quality of care, and one of the most important aspects of good patient access is good communication between patients and healthcare providers. Research documents show a direct relationship between patient compliance and quality of care.
What does patient access mean to you?
At its most basic, “patient access” is defined quite literally. It refers to the availability of healthcare, the ability of consumers to access care and treatment. Patient access is an integral part of the Affordable Care Act (ACA).
What is non compliance with medication?
The term “non-compliance” might be taken to refer both to the failure to follow a drug regimen and to the failure to adopt other measures that contribute to improvement in health—for example, changes in lifestyle or diet.
What impact would non compliance have on patients?
Noncompliance (non-adherence) to medical recommendations can have a significant impact on a patient's overall health quality, resulting in decreased opportunities for prevention, delayed diagnosis, and incomplete or ineffective treatment.
How do you handle noncompliant patients?
5 Tips for Treating Non-Compliant PatientsBe understanding. Put yourself in the patient's shoes and make every effort to be empathetic, thus recognizing the challenges they may experience when trying to understand your requests. ... Educate. ... Document everything. ... Set boundaries and enforce them. ... Avoid ultimatums.
Why don t hospitals let you take your own medicine?
Bringing your own medications from home and taking them while in the hospital has resulted in hundreds of medication errors over the years. If you bring your own medicines to the hospital, give them to the nurse.
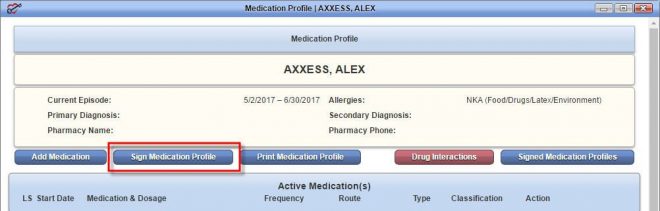
Which of the following must be included in a patient's medication list?
"It should list any allergies you have, prior adverse reactions and most importantly, include any current medications, with dosage and frequency, that you are taking," notes Dr. Hicks. The medication list should also include non-prescription medications such as supplements, aspirin, vitamins, and minerals.
How Medicare covers self administered drugs given in hospital outpatient settings?
If you get self-administered drugs that aren't covered by Part B while in a hospital outpatient setting, the hospital may bill you for the drug. However, if you're enrolled in a Medicare drug plan (Part D), the plan may cover these drugs.
What is patient access process?
Patient Access typically involves scheduling, registration, financial clearance, and patient collection.
What is patient access for a biotech?
Patient access is a mindset that focuses on providing patients with access to the medicines they need at acceptable prices. Providing patients with access is the one common goal all stakeholders can agree on.
What are the process involved in patient access?
Patient Access ServicesSchedule Patients and obtain all patient details.Verify Insurance, and eligibility for services - determine copayment, Co-insurance and deductible levels.Determine prior authorization requirements.Register Patients- make demographic and insurance updates.
Why is patient Access important in healthcare?
Patient Access often sets the tone for the patient's perception of the organization and their overall care journey. Consumers of health care are looking for the same conveniences, access to information and customer service that they are used to from other industries, such as retail and travel.
Medication Adherence: The Ultimate Guide For 2022 - Ōmcare
Limited health literacy. Nearly 36% of people in America have very little health literacy. This means that they don’t possess a good understanding of their health plan or healthcare in general, and thus cannot make educated decisions about their bodies.
Medication Adherence Tools | McKesson
Medication adherence, sometimes called medication compliance, is when a patient takes their prescription drug correctly: on time, in the correct dosage and for the length of time their doctor prescribed.
Interventions to Improve Medication Adherence: A Review
Importance: Among adults with chronic illness, 30% to 50% of medications are not taken as prescribed. In the United States, it is estimated that medication nonadherence is associated with 125 000 deaths, 10% of hospitalizations, and $100 billion in health care services annually.
Strategies and Emerging Interventions for Improving Medication Adherence
The authors identified 30 easily accessible apps that had some of the following features: medication lists, reminders and refill alerts, education, secure networks, and
Do You Know the Difference Between These Adherence Measures?
This is a relatively simple calculation, but it has its faults. For instance, MPR can overestimate adherence, and in many cases, it does. Patients who routinely refill their medications early will have an inflated MPR, as the numerator in this equation will be larger than the denominator.
Who must obtain prior authorization from the Medicaid agency?
A physician who wishes to prescribe medications that do not appear on the PDL (or formulary) must obtain prior authorization from the Medicaid agency (or its subcontractor) to allow the patient to obtain the drug medications through the Medicaid program.
What is a restrictive formulary?
In the early 1990s, states used drug formularies (lists of medications) to limit Medicaid beneficiaries' access to medications. Many of these formularies contained only one or two mental health medications and rarely did they include the newest or most effective drugs available.
What is behavioral pharmacy management system?
Behavioral Pharmacy Management Systems were initiated in Missouri and Pennsylvania in the early 2000's. They involve a software program which reviews Medicaid pharmacy claims against an evidence-based algorithm for mental health medications to identify "outlier" prescribing patterns that fall outside of clinically recommended practices , such as multiple antipsychotics or unusually high or low doses of medications. Prescribers with unusual patterns are sent information designed to improve prescribing. The software can be customized to elicit prescribing patterns which are of particular concern to a given state. In addition, informational packets may be followed by "peer to peer" education calls regarding evidence-based guidelines and best practices, particularly if the initial effort failed to change a prescriber's habits.
How does a case management program help?
A similar strategy is Prescription Case Management programs, which help monitor and ensure appropriate medication usage - often for a targeted population - through joint clinical reviews when prescribing activity is unusually high or outside of usual clinical practice. A good is example is the North Carolina Nursing Home Polypharmacy Initiative, in which a state physician/pharmacist team reviews the cases of nursing home residents who take more than 18 medications in 90 days and then makes recommendations to improve care. In 2002, the state's nursing homes carried out 74 percent of team recommendations, improving the health of their residents and savings the state $16 million in drug costs.
When did Medicaid start charging nominal fees?
When Medicaid was first instituted in 1965, states were not permitted to charge beneficiaries for covered services. However, that changed in 1972 when the federal government allowed states to charge nominal fees for services to medically needy beneficiaries.
How did cost sharing affect health care?
Even countries with national health insurance programs have tried to implement cost-sharing and the subsequent research demonstrated barriers to care. In 1996, Quebec imposed co-payments for prescription drugs on more than 100,000 welfare recipients. The researchers found that after the imposition of co-payments, the beneficiaries filled fewer prescriptions for essential medications. The co-payments led to a 78% increase in the occurrence of adverse events, including death, hospitalization, and nursing home admissions. Co-payments also led to an 88% increase in emergency room use. (R. Tamblyn, R. Laprise, J. Hanley, et al., "Adverse Events Associated with Prescription Drug Cost-Sharing among Poor and Elderly Persons, "Journal of the American Medical Association, 285 (4), January 2001).
Who should have input into the process and review of documents?
In addition, advocates, consumers, family members and providers should have input into the process and review of documents. This requires that notice of meetings, proposed policy changes, policy changes under consideration and other relevant issues needs to be made available to the public well in advance.
What is non-adherence in healthcare?
Non-adherence used to be called “noncompliance, ” and that term is still heard occasionally but implies a willful refusal to do what they should do, and health care providers are increasingly recognizing that outside factors are often to blame.
Why don't people take their medications?
While all of these are factors, there is one big reason people don’t take their medications: cost. Out-of-pocket costs for prescription medications have been rising steadily, faster than inflation or health spending overall .
What percentage of prescriptions aren't filled?
Experts estimate that up to 50 percent of medications that physicians prescribe to their patients don’t end up being taken as directed. At least 20 percent of the prescriptions aren’t even filled.
How many people die from not following prescriptions?
Failure to follow prescriptions causes some 125,000 deaths a year and up to 10 percent of all hospitalizations. Medication non-adherence can have a number of causes: patients don’t like the side effects, or their lack of symptoms makes them think they don’t need the drugs anymore.
How much does non-adherence cost?
This non-adherence leads to hospitalizations when chronic conditions flare up, and these hospitalizations cost the health care system between $100 billion and $289 billion each year.
How much is a 90 day supply of generic drugs?
Even if you have insurance, don’t always assume that rate will be better; some stores offer a 30-day supply of certain generic drugs for $4 (and a 90-day supply for $10), and this price is likely to be better than the copay of your insurance.
Do pharmacists know if you're taking a pill?
Pharmacists are in a perfect position to know whether patients have been taking their pills regularly , and they can offer assistance when they see someone hasn’t been filling their prescriptions. “There are a number of competing demands,” Sharkey said.
What are the barriers to medication adherence?
Tailored pharmacy-based interventions address barriers to medication adherence by examining the factors that affect a person’s ability to take their medications. These barriers may be complex and include factors related to socioeconomics, health care system structures and processes, severity of co-occurring medical conditions, complexity of medication and nonmedication therapies, and patient concerns. 3
What is medication management?
Medication therapy management (MTM)9 includes a broad range of health care services provided by pharmacists—the medication experts on a patient’s health care team. It allows pharmacists to actively manage patients’ medications and identify, prevent, and resolve medication-related problems. This support helps patients get the most benefit from their medications. MTM services include medication therapy reviews, pharmacotherapy consults, anticoagulation management, immunizations, health and wellness programs, and many other clinical services.
What is the Joint Commission of Pharmacy Practitioners?
The Joint Commission of Pharmacy Practitioners developed the Pharmacists’ Patient Care Process#N#external icon#N#to address medication nonadherence for chronic diseases. Steps in the process (collect, assess, plan, implement, follow-up, and monitor) closely align with how a pharmacist selects tailored actions to remove or reduce patient adherence barriers.
How does a pharmacy intervention help with CVD?
Tailored pharmacy-based interventions to improve medication adherence among patients with CVD risk factors help address growing health care costs. These interventions lead to cost savings from reductions in outpatient primary care and specialist visits , hospitalizations, and emergency department use. 18 The full economic impact of implementing these interventions for key partners and participants involved in the delivery, payment, and receipt of these interventions have been largely unexplored by researchers.
How can public health practitioners support the CPSTF recommendation?
Public health practitioners and state and local health departments can support use of the CPSTF recommendation by promoting and helping pharmacies implement tailored pharmacy-based interventions.
Why is it important to recognize and convene partners involved in implementing the interventions?
As state and local health departments consider introducing or expanding these interventions in their communities, an important first step is to recognize and convene partners involved in implementing the interventions to ensure greater efficiencies, better health, and cost savings. By considering each key player’s role in terms of potential costs and benefits, state and local health departments and their partners may better understand how each may facilitate their implementation and be affected by them.
Why are pharmacies using the Patient Care Process?
These stories describe how health systems and pharmacies in select communities across the country are using the Pharmacists’ Patient Care Process to help their patients prevent and control chronic conditions, including high blood pressure.
Who owns mental health records?
While mental health treatment records are owned by the practitioner (assuming a private practitioner/sole proprietorship), patients have certain rights with respect to accessing their treatment records. These rights are typically specified by state statute, but for those who are “covered entities” under HIPAA these rights are found in ...
What are HIPAA rights?
These rights are typically specified by state statute, but for those who are “covered entities” under HIPAA these rights are found in the federal regulations known as the Privacy Rule. Patients or clients may gain access to their records by either obtaining a copy of the records or by inspecting the records. From the practitioner’s standpoint, ...
Can a mental health practitioner deny access to records?
Under specified circumstances, access to the records either may or must be denied. The grounds for a denial may vary when state law is compared to the Privacy Rule. In order to deny access in California, the practitioner must determine that there is a substantial risk of significant adverse or detrimental consequences to a patient in seeing or receiving a copy of the mental health records requested by the patient. The law then specifies several other actions that the practitioner must take, including what content must be entered into the records. For those who are covered entities under HIPAA, the standard for denial is worded differently (e.g., but not limited to, where access is reasonably likely to endanger the life or physical safety of the individual or another person). Some denials of access by the practitioner (under HIPAA) are not reviewable (e.g., denial of access to “psychotherapy notes”), while other denials are reviewable. When denying access under the Privacy Rule, the practitioner must, among other things, provide a timely, written denial that contains the basis for the denial and information regarding the review rights for the individual seeking access.
Can a patient consent to a summary?
Sometimes, after thoughtful discussion and reasoning, patients may consent to a summary.
Can a minor's parent inspect a minor's medical records?
With respect to parental access to a minor’s records, California law specifies that the representative of a minor “ shall not be entitled to inspect or obtain copies of the minor’s patient records” under two circumstances.
Do practitioners have to know the laws?
While practitioners are expected to know the laws and regulations that affect their profession, there are some practical limitations and nuances (like vague and ambiguous laws, or conflicts between federal and state law) that essentially prevent or hamper practitioners from knowing everything that they should.
Can a summary of a medical record be provided in California?
Under HIPAA regulations (the Privacy Rule), a summary can only be provided if the patient agrees in advance to a summary and to the reasonable, cost-based fee imposed, if any, by the practitioner for preparation of the summary. For those governed by state law, more latitude may be given to the practitioner. In California, for example, a summary of the records may be provided in the discretion (hopefully, the sound discretion) of the practitioner. There are no findings that first have to be made and no conditions that first have to be met (California may be alone in this regard). When provision of a summary is permitted, whether in the sole discretion of the practitioner or under specified conditions, it is important to know whether there is specific content that must be contained in the summary and what that content is. In California, the relevant statute lists at least eight specific things that must be included in a summary of the records.
When did the US start providing free prescriptions?
Recognizing that more funding is needed to help financially needy patients get access to the most effective medicines for their conditions, in the 1990s US drug manufacturers created prescription assistance and access programs as a way to give free or reduced-cost branded medications to those patients who could not afford them. At that time, the approach was simple: drug manufacturers provided their medicines at no or low cost to patients who could not afford to buy them based on the decision of the prescribing clinician.
Why are PAPs important?
The reasoning is that PAPs shield patients from the economic effects of drug pricing and discourage generic drug use, despite the fact that many of these programs cover medicines that do not have generic versions.
Where is the greatest rate of access to new medicines?
Patient access to new medicines is highly varied across Europe, with the greatest rate of availability in Northern and Western European countries and lowest in Southern and Eastern European countries.
How long does it take to get a new product after a patient has been approved?
The average delay between market authorization and patient access can vary by a factor greater than seven-fold across Europe, with patients in Northern/Western Europe accessing new products from 100-200 days after market authorization, but 600-1000 days from market authorization for patients mainly in Southern/Eastern Europe .
What is the W.A.I.T. indicator?
Examining disparities in the speed of access and availability of new medicines is the focus of EFPIA’s W.A.I.T. Indicator report. Everyone involved in healthcare–from patients to service providers, from researchers to clinicians, and from pharmaceutical companies to payers–wants to see patients across Europe get access to new treatment options. This report is designed to provide an accurate picture of the realities of access to medicines in Europe. It’s our hope that by focusing on the needs of patients and working with partners across healthcare we can find collaborative solutions to address the issues raised in this report.
Does availability indicate uptake?
The rate of availability in a country does not necessarily indicate medicine uptake, as some medicines may be available in a market with no uptake (no sales or no volume).
Is egulatory approval necessary for drug launch?
egulatory approval (marketing authorization) is necessary for drug launch but is not sufficient to guarantee patient access to a licensed medicine. There is a time lag between a marketing authorization and patient access. The question of how long that lag is matters a great deal to patients.
What are the barriers to medication adherence?
Tailored pharmacy-based interventions address barriers to medication adherence by examining the factors that affect a person’s ability to take their medications. These barriers may be complex and include factors related to socioeconomics, health care system structures and processes, severity of co-occurring medical conditions, complexity of medication and nonmedication therapies, and patient concerns. 3
What is medication management?
Medication therapy management (MTM)9 includes a broad range of health care services provided by pharmacists—the medication experts on a patient’s health care team. It allows pharmacists to actively manage patients’ medications and identify, prevent, and resolve medication-related problems. This support helps patients get the most benefit from their medications. MTM services include medication therapy reviews, pharmacotherapy consults, anticoagulation management, immunizations, health and wellness programs, and many other clinical services.
What is the Joint Commission of Pharmacy Practitioners?
The Joint Commission of Pharmacy Practitioners developed the Pharmacists’ Patient Care Process#N#external icon#N#to address medication nonadherence for chronic diseases. Steps in the process (collect, assess, plan, implement, follow-up, and monitor) closely align with how a pharmacist selects tailored actions to remove or reduce patient adherence barriers.
How does a pharmacy intervention help with CVD?
Tailored pharmacy-based interventions to improve medication adherence among patients with CVD risk factors help address growing health care costs. These interventions lead to cost savings from reductions in outpatient primary care and specialist visits , hospitalizations, and emergency department use. 18 The full economic impact of implementing these interventions for key partners and participants involved in the delivery, payment, and receipt of these interventions have been largely unexplored by researchers.
How can public health practitioners support the CPSTF recommendation?
Public health practitioners and state and local health departments can support use of the CPSTF recommendation by promoting and helping pharmacies implement tailored pharmacy-based interventions.
Why is it important to recognize and convene partners involved in implementing the interventions?
As state and local health departments consider introducing or expanding these interventions in their communities, an important first step is to recognize and convene partners involved in implementing the interventions to ensure greater efficiencies, better health, and cost savings. By considering each key player’s role in terms of potential costs and benefits, state and local health departments and their partners may better understand how each may facilitate their implementation and be affected by them.
Why are pharmacies using the Patient Care Process?
These stories describe how health systems and pharmacies in select communities across the country are using the Pharmacists’ Patient Care Process to help their patients prevent and control chronic conditions, including high blood pressure.