See more

What will the interoperability and patient access regulation allow a customer to do?
The Interoperability and Patient Access final rule (CMS-9115-F) delivers on the Administration's promise to put patients first, giving them access to their health information when they need it most and in a way they can best use it.
How does interoperability impact patient care?
By helping to ensure that data exchanged between two devices is captured and interpreted accurately, interoperable clinical accessories can reduce the risk of preventable errors and serious inefficiencies, which is beneficial to the materials management team, clinicians, and patients.
What is CMS interoperability program?
In 2011, CMS established the Medicare and Medicaid EHR Incentive Programs (now known as the Medicare Promoting Interoperability Program) to encourage EPs, eligible hospitals, and CAHs to adopt, implement, upgrade, and demonstrate meaningful use of certified electronic health record technology (CEHRT).
Who regulates interoperability in healthcare?
Information & Tools: The CMS Interoperability and Patient Access final rule requires CMS-regulated payers to implement and maintain a secure, standards-based Patient Access API (using Health Level 7® (HL7) Fast Healthcare Interoperability Resources® (FHIR) 4.0.
What are the benefits of interoperability in healthcare?
5 key benefits of interoperabilityInformed decision making. Greater levels of access to real-time patient data from key health or care agencies aids more accurate treatments. ... Efficient patient care. ... Transfer of care. ... Availability of comprehensive patient information. ... Improving the patient experience.
What is an example of interoperability in healthcare?
Levels Of Interoperability An example might be the use of a patient portal to send a PDF document that has patient history information. The recipient of the PDF document would need to open it and manually enter that data into an electronic medical record system.
What is patient Access API?
The Patient Access API is used to build applications that enable HCSC customers to easily access their claims and encounter information, including cost, as well as a defined sub-set of their clinical information. This is a RESTful API that conforms to the FHIR standard and provides access to HCSC customer data.
What are CMS guidelines?
CMS regulations establish or modify the way CMS administers its programs. CMS' regulations may impact providers or suppliers of services or the individuals enrolled or entitled to benefits under CMS programs.
What impact do you think that the promoting interoperability programs has on healthcare organizations and patients?
Interoperability helps keep patient data more secure because of how it limits the need for manual data transcription and copying. Your staff will tend to work more productively when the computer systems are set up for maximum interoperability, with databases and other applications connecting and sharing information.
What are the four levels of interoperability?
There are four levels of interoperability: foundational, structural, semantic, and organizational. Foundational interoperability is the ability of one IT system to send data to another IT system.
What is CMS interoperability in healthcare?
CMS Interoperability and Prior Authorization Proposed Rule This proposed rule emphasizes the need to improve health information exchange to achieve appropriate and necessary access to complete health records for patients, health care providers, and payers.
What are interoperability requirements?
In the sea of non-functional requirements, interoperability is defined as how easily a system can share information and exchange data with other systems and external hardware.
What does CMS stand for?
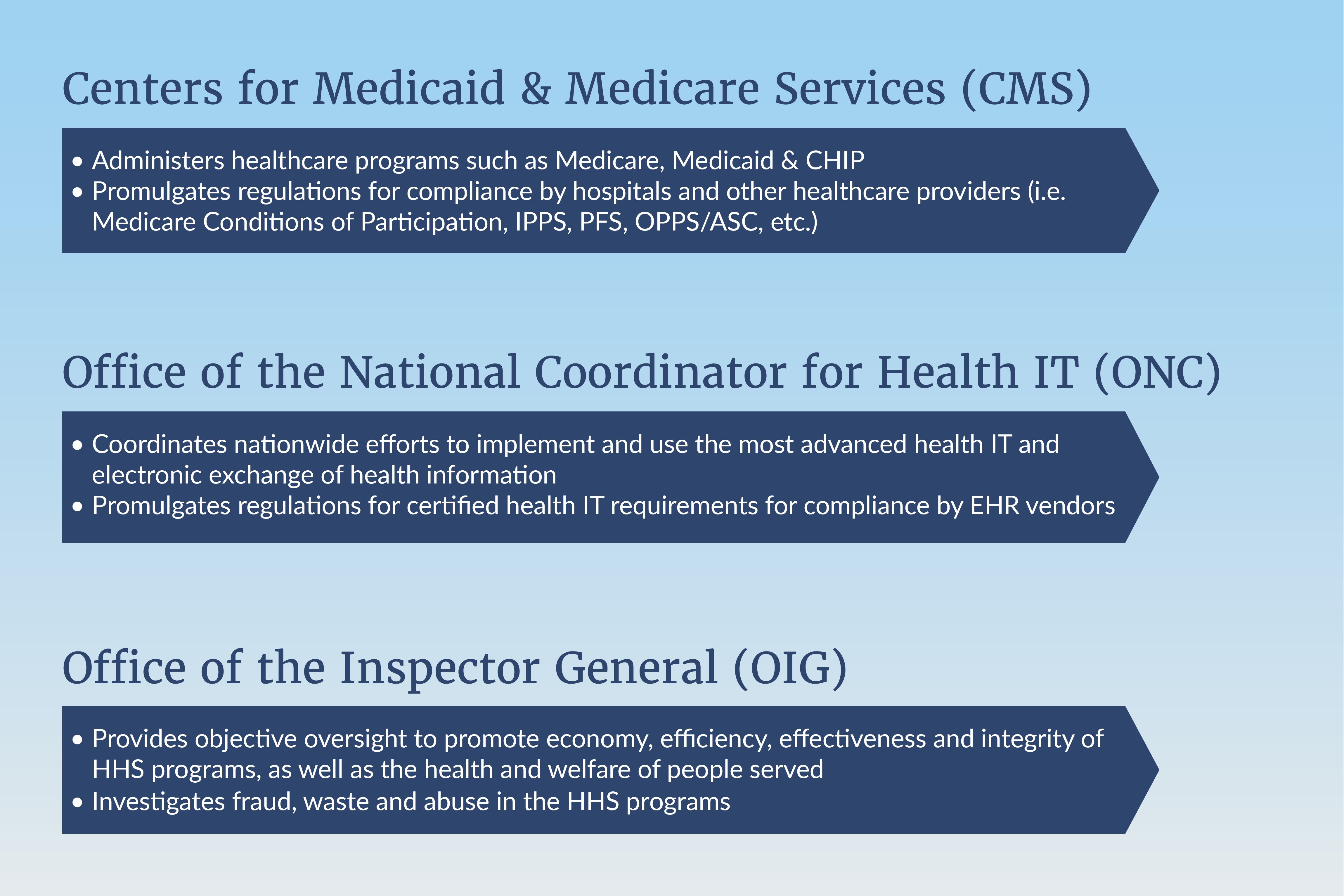
Centers for Medicare & Medicaid ServicesThe Centers for Medicare & Medicaid Services, CMS, is part of the Department of Health and Human Services (HHS).
What are the 4 main goals of the meaningful use program?
They were: Improve quality, safety, efficiency, and reduce health disparities.
What are the 3 stages of meaningful use?
Stages of Meaningful Use The meaningful use objectives will evolve in three stages: Stage 1 (2011-2012): Data capture and sharing. Stage 2 (2014): Advanced clinical processes. Stage 3 (2016): Improved outcomes.
What are interoperability requirements?
In the sea of non-functional requirements, interoperability is defined as how easily a system can share information and exchange data with other systems and external hardware.
When will CMS enforce interoperability and patient access?
As of July 1, 2021, two of the policies from the May 2020 Interoperability and Patient Access final rule are now in effect. On April 30, 2021, the requirements for hospitals with certain EHR capabilities to send admission, discharge and transfer notifications to other providers went into effect. On July 1, 2021, CMS began to enforce requirements for certain payers to support Patient Access and Provider Directory APIs. Additional information is available on the FAQ page and in the other information available below.
What is CMS interoperability?
When implemented effectively, health information exchange (interoperability) can also reduce the burden of certain administrative processes, such as prior authorization.
What is FHIR release 4.0.1?
FHIR Release 4.0.1 provides the first set of normative FHIR resources. A subset of FHIR resources is normative, and future changes on those resources marked normative will be backward compatible. These resources define the content and structure of core health data, which developers to build standardized applications.
What are IGs used for?
These guides provide information payers can use to meet the requirements of CMS rules without having to develop an independent approach, which will save time and resources. In addition, the reference implementations available on the applicable websites allow payers to see the APIs in action and support testing and development.
What is CMS Interoperability and Patient Access Final Rule?
In August 2020, CMS released a letter to state health officers detailing how state Medicaid agencies should implement the CMS Interoperability and Patient Access final rule in a manner consistent with existing guidance. There are many provisions in this regulation that impact Medicaid and CHIP Fee-For-Service (FFS) programs, Medicaid managed care plans, and CHIP managed care entities, and this letter discusses those issues. Additionally, this letter advises states that they should be aware of the ONC’s 21st Century Cures Act final rule on information blocking. The link for the letter is:
What is CMS 9115-F?
The Interoperability and Patient Access final rule (CMS-9115-F) put patients first by giving them access to their health information when they need it most, and in a way they can best use it. This final rule focused on driving interoperability and patient access to health information by liberating patient data using CMS authority to regulate Medicare Advantage (MA), Medicaid, Children's Health Insurance Program (CHIP), and Qualified Health Plan (QHP) issuers on the Federally-facilitated Exchanges (FFEs).
What is the payer requirement?
Payers are required to make a patient’s claims and encounter data available via the Patient Access API.
What is CMS Interoperability and Patient Access Final Rule?
In August 2020, CMS released a letter to state health officers detailing how state Medicaid agencies should implement the CMS Interoperability and Patient Access final rule in a manner consistent with existing guidance. There are many provisions in this regulation that impact Medicaid and CHIP Fee-For-Service (FFS) programs, Medicaid managed care plans, and CHIP managed care entities, and this letter discusses those issues. Additionally, this letter advises states that they should be aware of the ONC’s 21st Century Cures Act final rule on information blocking. The link for the letter is:
What is interoperability in healthcare?
When implemented effectively, health information exchange (interoperability) can also reduce the burden of certain administrative processes, such as prior authorization. We have issued regulations that will drive change in how clinical and administrative information is exchanged between payers, providers and patients, and will support more efficient care coordination.
What is FHIR release 4.0.1?
FHIR Release 4.0.1 provides the first set of normative FHIR resources. A subset of FHIR resources is normative, and future changes on those resources marked normative will be backward compatible. These resources define the content and structure of core health data, which developers to build standardized applications.
What is OpenID Connect 1.0?
OpenID Connect 1.0 is a simple identity layer on top of the OAuth 2.0 protocol. It enables clients to verify the identity of the end-user based on the authentication performed by an authorization server, as well as to obtain basic profile information about the end-user in an interoperable and RESTful manner. This specification defines the core OpenID Connect functionality: authentication built on top of OAuth 2.0 and the use of claims to communicate information about the end-user. It also describes the security and privacy considerations for using OpenID Connect.
What is CMS 9115-F?
The Interoperability and Patient Access final rule (CMS-9115-F) put patients first by giving them access to their health information when they need it most, and in a way they can best use it. This final rule focused on driving interoperability and patient access to health information by liberating patient data using CMS authority to regulate Medicare Advantage (MA), Medicaid, Children's Health Insurance Program (CHIP), and Qualified Health Plan (QHP) issuers on the Federally-facilitated Exchanges (FFEs).
What is the payer requirement?
Payers are required to make a patient’s claims and encounter data available via the Patient Access API.
When will CMS start enforcing the API?
CMS began enforcing these new requirements on July 1, 2021.
What is a CMS regulated health plan?
CMS-regulated health plans must enable patients to be able to access and share their health data through a FHIR-based API.
Can CMS regulated health plans share clinical data?
CMS-regulated health plans must be able to share clinical data (USCDI v1) with other health plans upon a members request.
What is CMS looking for?
Together with the Office of the National Coordinator for Health Information Technology (ONC), CMS is requesting feedback on how it can leverage its authority to improve patient identification and safety to encourage better coordination of care across different healthcare settings while advancing interoperability.
How does CMS improve healthcare?
The RFIs continue the national conversation about improving the healthcare delivery system and includes how CMS can: 1 Promote interoperability 2 Reduce burden for clinicians, providers, and patients, while encouraging care coordination, and 3 Lead change to a value-based healthcare system.
What is Medicaid data exchange?
The data exchanged include files of all eligible Medicaid beneficiaries by state, as well as “buy-in” data, or information about beneficiaries states are using Medicaid funds to “buy-in” Medicare services.
What is CMS model testing?
CMS plans to promote interoperability across the healthcare spectrum through model testing that focuses on using emerging standards, models leveraging non-traditional data and technology-enabled patient engagement platforms.
What should commenters provide CMS with?
In responding to the RFIs, commenters should provide CMS with clear and concise proposals that include data and specific examples. Analysis regarding CMS’ authority is welcome, particularly if proposals involve novel legal questions. CMS will not respond to RFI comment submissions in the final rule, but will actively consider all input in developing future regulatory proposals and/or sub-regulatory guidance.
What is the Innovation Center?
The Center for Medicare and Medicaid Innovation ("Innovation Center") models are an important lever to advance interoperability. The Innovation Center is seeking public comment on promoting interoperability among model participants and other healthcare providers as part of the design and testing of innovative payment and service delivery models.
What is CMS Interoperability and Patient Access?
The CMS Interoperability and Patient Access final rule requires CMS-regulated payersto implement and maintain a secure, standards-based Patient Access API (using Health Level 7® (HL7) Fast Healthcare Interoperability Resources® (FHIR) 4.0.1)that allows patients to easily access their claims and encounter information, including cost, as well as a defined sub-set of their clinical information through third-party applications of their choice. This rule also requires MA organizations, Medicaid FFS programs, CHIP FFS programs, Medicaid managed care plans, and CHIP managed care entities to make provider directory information publicly available via a FHIR-based Provider Directory API.
When will the CMS Interoperability and Patient Access final rule be effective?
Recognizing that hospitals, including psychiatric hospitals, and critical access hospitals, are on the front lines of the COVID-19 public health emergency, CMS is extending the implementation timeline for the admission, discharge, and transfer (ADT) notification Conditions of Participation (CoPs) by an additional six months to be effective May 1, 2021 (date the final rule was published in the Federal Register).
What is CMS 9115-F?
As part of the Trump Administration’s MyHealthEData initiative, the Interoperability and Patient Access final rule (CMS-9115-F) is focused on driving interoperability and patient access to health information by liberating patient data using CMS authority to regulate certain health plan issuers on the Federally-facilitated Exchanges (FFEs).
When will CMS interoperability mandates be implemented?
CMS recently introduced new interoperability mandates for health plans that must be implemented by July 1, 2021. This rule is designed to make health information more easily available to patients by implementing new industry standards like HL7 FHIR APIs and by deterring information blocking. The CMS Interoperability and Patient Access final ...
What is patient privacy and security resources?
Patient Privacy and Security Resources – Supporting Payers Educating their Patients
What are the three technical standards for the 21st Century Cures Act?
These are FHIR, SMART IG/OAuth 2.0, OpenID Connect, and USCDI , respectively. Implementation Guidance:
Is the Patient Access API mandatory?
The use of these guides is not mandatory, but using these guides can help payers save both time and resources.